Hip osteoarthritis (often called hip arthritis) is one of the most common causes of hip pain in adults over 50. It affects not just the joint itself but also a person’s mobility, confidence, and quality of life.
As physiotherapists, we are often asked:
- What actually is hip osteoarthritis?
- Why does it happen?
- What’s the best treatment—can physio really help, or is surgery inevitable?
This blog breaks down the current research on hip osteoarthritis and explains what it means for people living with hip pain.
What is Hip Osteoarthritis?
The old view of osteoarthritis (OA) is that is is just “wear and tear.” The more up-to-date, modern view is that it is a whole joint and whole person condition, with many factors contributing to the end pain experience:
- Osteoarthritis affects cartilage (the smooth tissue that cushions the bones), bone, ligaments, muscles, and even the synovium (the lining of the joint).
- It’s driven by a mix of inflammation, mechanical stress, and reduced ability to repair damage, which leads to gradual joint changes.
- Pain is influenced not only by the joint changes but also by lifestyle, mental health, sleep and activity levels.
About 1 in 4 people over 85 experience symptomatic hip OA, and around 10% of people will eventually need a total hip replacement for end-stage disease. 90% will be able to manage their symptoms and maintain a good quality of life without th need for surgical intervention.
Symptoms of Hip Osteoarthritis
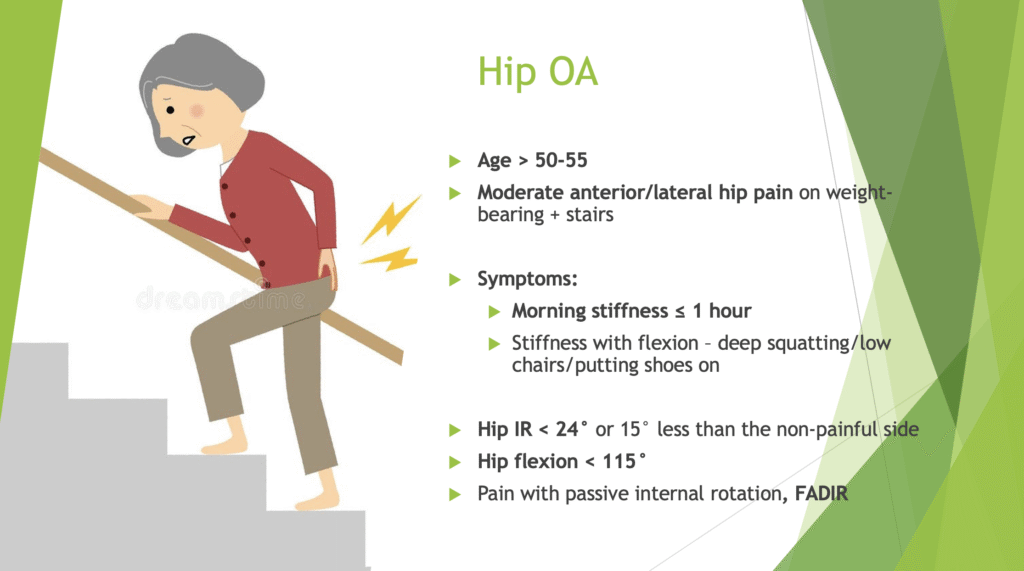
Common signs include:
- Hip or groin pain that worsens with weight-bearing (standing, walking, stairs).
- Morning stiffness (usually less than an hour).
- Difficulty with deep squatting, low chairs, or putting on shoes/socks.
- Reduced movement, especially internal rotation of the hip.
If you’re over 50 and have these symptoms, hip OA could be the cause.
Why Does Hip Osteoarthritis Happen?
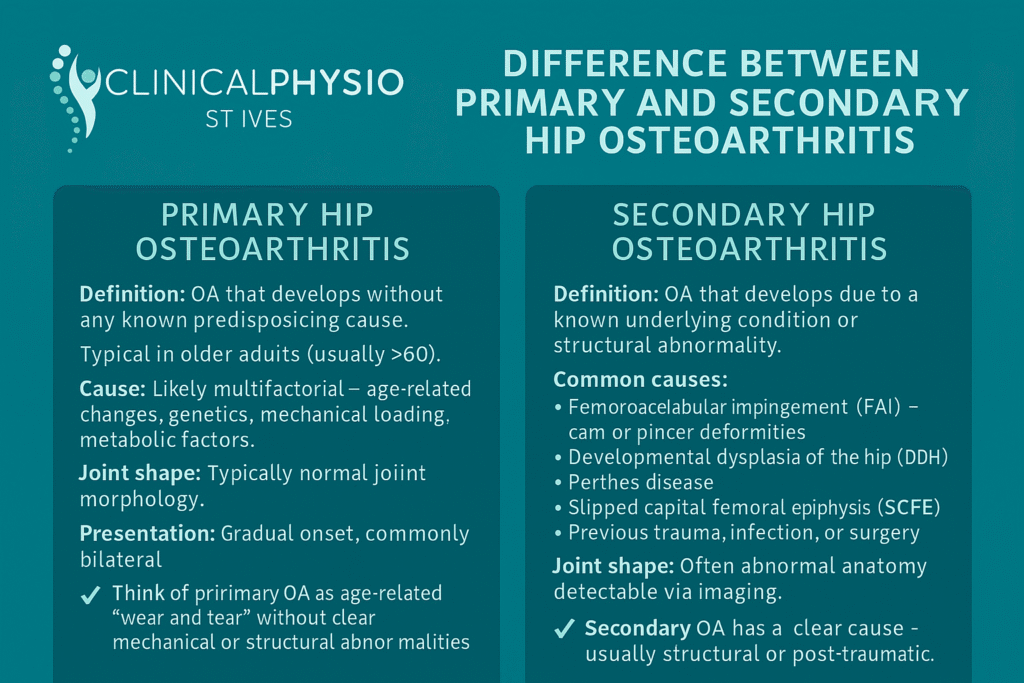
Hip OA can be primary (developing without a clear cause, usually age-related) or secondary (caused by another problem). The table below shows the difference between the two types.
Risk factors include:
- Age – risk increases after 50.
- Genetics – studies show up to 60% of hip OA risk is inherited.
- Body weight – each 5-point increase in BMI increases risk by about 11%.
- Occupation – heavy manual work (e.g., farming) raises risk more than threefold.
- Sports – high-impact activities in adolescence (like football or hockey) may alter hip shape and increase OA risk.
- Hip shape – conditions such as femoroacetabular impingement (FAI) or hip dysplasia create abnormal joint loading and double the risk of hip arthritis.
How is Hip Osteoarthritis Diagnosed?
Contrary to popular belief, hip osteoarthritis does not require on x-ray for diagnosis. Diagnosis is made using the following criteria:
- Age = >50
- Symptoms = pain in the hip/groin region, stiffness, reduced mobility).
- Physical examination = reduced range of motion of hip flexion and internal rotation
Importantly, X-ray findings don’t always match pain levels. Some people with severe changes feel little pain, while others with mild changes can have significant symptoms.
Evidence-Based Hip Osteoarthritis Treatment (See references below)
The good news is that physiotherapy for hip arthritis is one of the most effective first-line treatments. Research consistently shows that exercise and education can reduce pain, improve mobility, and delay or even prevent surgery.
1. Education and Self-Management
- Understanding OA helps reduce fear (“it’s not just bone-on-bone”).
- Learning pacing strategies and flare-up management empowers patients.
- Shared decision-making ensures treatment matches your goals.
2. Exercise Therapy (Best Evidence)
Exercise is the cornerstone of hip osteoarthritis treatment. Exercises should be tailored to the exact deficits that are found during an assessment. Some common areas that are targeted are:
- Strengthening the hip and pelvic muscles including hip abductors (like gluteus medius), hip adductors (like adductor longus) and hip extensors (like gluteus maximus and the hamstrings).
- Improving movement control and flexibility.
- Increasing fitness, which reduces inflammation and helps weight management.
Programs like GLA\:D® (Good Life with Osteoarthritis in Denmark) is a popular program and can be helpful for those with moderate symptoms. However, the GLAD program is yet to be studied in a randomised control trial that compares it to other exercise and education interventions and isn’t tailored to address individual, patient-specific deficits.
3. Manual Therapy
Joint mobilisations and soft tissue techniques can provide short-term relief when combined with exercise.
4. Weight Management and Lifestyle Factors
Even modest weight loss can reduce joint stress and improve symptoms. Supportive footwear and walking aids may also help reduce load.
5. Other Options
- Injections: Corticosteroid injections may provide temporary relief (1–8 weeks), but repeated use is discouraged. Hyaluronic acid and PRP (platelet-rich plasma) currently have limited evidence.
- Surgery: Total hip replacement (THR) is highly effective for end-stage hip OA, with over 90% of patients reporting major pain relief and excellent implant survival rates. However, for many people, good physiotherapy can delay or even avoid the need for surgery.
Key Takeaways
- Hip OA is common and not just wear and tear—it’s a whole-joint condition influenced by multiple factors.
- Hip arthritis physio (exercise and education) is the best first-line treatment.
- Manual therapy, weight management, and injections can support recovery.
- Surgery is effective but should usually be considered only after conservative options are tried.
- A personalised, evidence-based approach gives the best results.
References
- Hall et al. (2022). How does hip osteoarthritis differ from knee osteoarthritis? Osteoarthritis & Cartilage.
- Casartelli et al. (2021). Is Hip Morphology a Risk Factor for Hip Osteoarthritis? A Systematic Review & Meta-Analysis.
- Skou & Roos (2019). Supervised, Active Treatment Is Current Best Practice. Clinical and Experimental Rheumatology.
- van Doormaal et al. (2020). Clinical practice guideline for physical therapy in hip and knee OA. Musculoskeletal Care.
- Murphy, Eyles & Hunter (2021). Hip Osteoarthritis: Etiopathogenesis and Management.
- Gibbs et al. (2023). Recommendations for the management of hip and knee osteoarthritis: A systematic review of clinical practice guidelines.


