Patellofemoral Pain Syndrome (PFPS) or “Runners Knee” is one of the most common overuse injuries amongst the active population. PFPS accounts for approximately 15% of all knee pain, with females and young adults being 2 times more likely to develop symptoms due to PFPS (Boling et al, 2010).
What is the Patello-Femoral Joint?
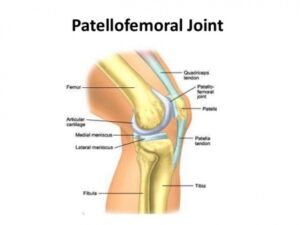
The Patello-femoral joint is one of two joints that make up the knee (see figure 1). It is comprised of the kneecap (patella) and the thigh bone (femur) and provides the attachment sites for our quadriceps and patella tendons.
How do I know if I have PFPS?
PFPS is characterised as “pain experienced around or behind the knee cap, which is aggravated by weight bearing activities that require a flexed knee such as squatting, running, jumping and hopping” (Crossley et al, 2016). It is not uncommon to also experience symptoms such as:
- Creaking/grinding sensations around the knee cap
- Swelling around the knee
- Pain provoked by pressing the knee cap
- Pain bought on by non-weight bearing activities such as sitting
How did I get PFPS?
Runners often develop PFPS due to a combination of several factors such as:
-
Muscular weakness (Quadriceps/Glutes)
-
Muscular tightness
-
Changes to training loads
-
Inappropriate footwear
-
Anatomical variations in knee cap shape/position
-
Changes to running style
-
Biomechanical abnormalities
What can I do to recover?
Currently, the best treatment supported by research is STRENGTH!!!
Strength interventions have been shown to be most effective in relieving pain and improving function in individuals with PFPS. Exercise selection should be patient specific and target the hip external rotators/hip abductors (Glut Medius) as well as the knee extensor muscles (Quadriceps) due to their roles in knee biomechanics (Martin et al, 2018).
The great news is approximately 90% of individuals suffering from PFPS will be completely symptom free within 6 weeks of starting a strength rehabilitation program guided by a physiotherapist.
What won’t work long term?
Amongst the literature there is a lack of strong evidence, supporting the long-term use of:
-
Electrical Stimulation
-
Ultrasound
-
TENS (Transcutaneous Electrical Nerve Stimulation)
-
Massage
-
Biofeedback devices
-
Taping
-
Orthotics
-
Dry needling
-
Acupuncture
Although the majority of these things can help your pain in the short term, none have been shown to be superior to strength exercises of the quadriceps and gluteal musculature.
It hurts to run….what can I do?
Research on running mechanics has shown that stress on the Patello-femoral joint is greatest during mid stance and exceeds approximately 7x your body weight. This can be largely increased with
-
Slower speeds of running (Increase knee flexion)
-
Large vertical oscillation
-
Cross over style running
-
Excessive body twisting
-
Excessive body twisting
Ways in which you can alter your running technique to reduce knee joint stress by 15-20% are:
-
Maintain space between your knees when running (knee window)
-
Increase running cadence by 10%
-
Minimise excessive body twisting
How can I prevent getting sore knees?
Currently the best evidence for preventing future patella issues besides maintaining your strength is by assessing and monitoring acute: chronic training volumes in term of distance covered (Km). Acute increases in training volume should be no greater than a factor of 1.5 or you place yourself at an increased risk of suffering a subsequent injury.
We have covered this in depth in our blog titled Our Top 3 injury prevention strategies, which can be accessed by the link below:
https://www.clinicalphysiostives.com.au/blogs/top-3-injury-prevention-strategies-lessons-from-leicester-city