SLAP Tear Management: Understanding and Rehabilitation Options for Shoulder Labral Injuries
If you’ve ever felt a deep, nagging shoulder pain when reaching overhead, throwing, or lifting weights, you may have heard the term SLAP tear mentioned. But what exactly does that mean — and how is it treated?
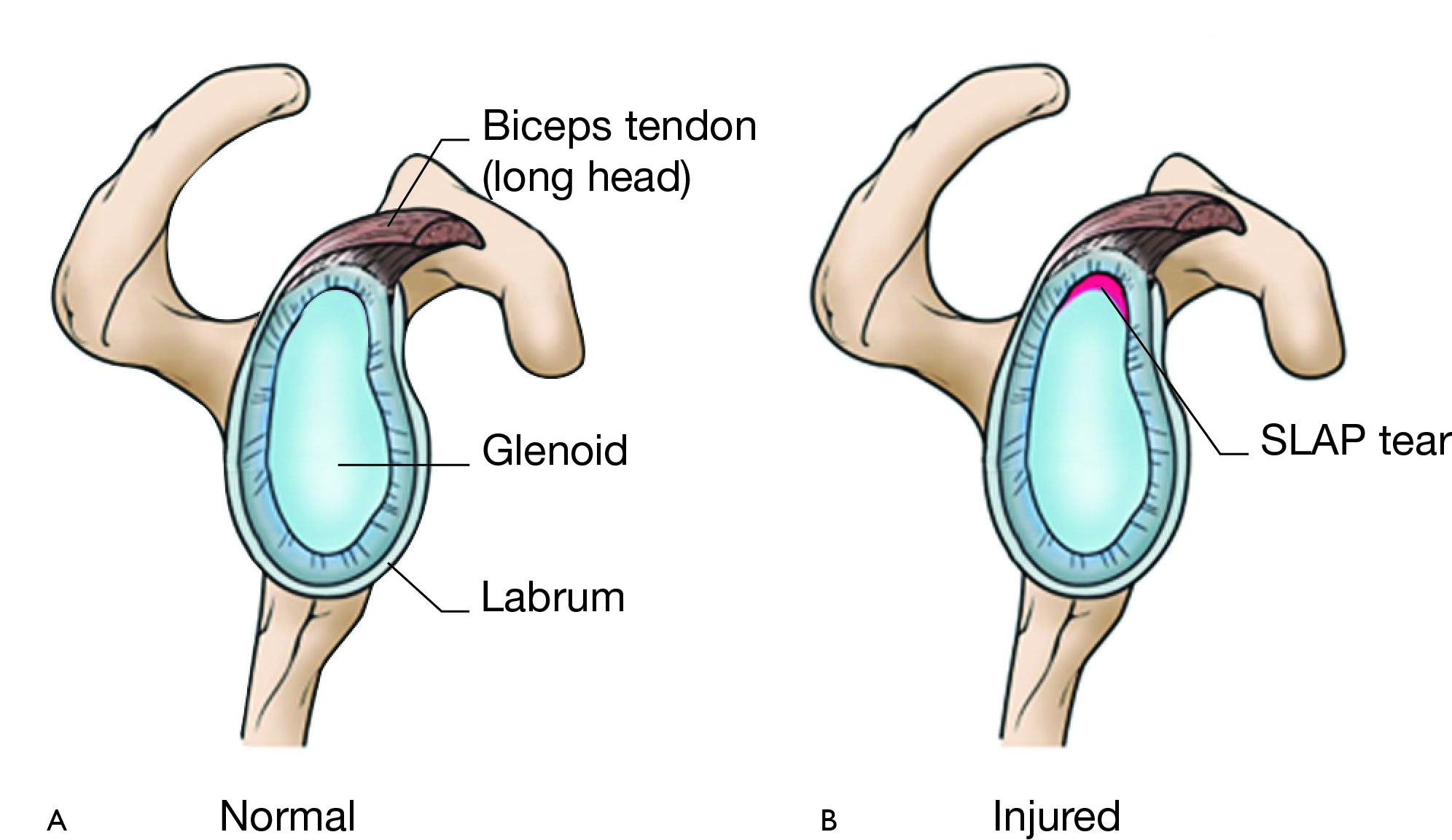
What is a SLAP Tear?
A SLAP tear stands for Superior Labrum Anterior to Posterior — meaning a tear of the top part of the shoulder’s labrum, where the biceps tendon attaches. The labrum is a ring of cartilage that deepens the shoulder socket, helping keep the joint stable and absorb forces during movement.
When this structure tears, it can cause pain deep in the joint, clicking or catching sensations, and loss of strength with overhead movements. SLAP tears are relatively uncommon, making up only about 5% of all shoulder problems, but they’re more frequent in overhead athletes such as tennis players, swimmers, baseballers, and tradies working with arms above shoulder height.
Interestingly, research shows that many people — especially those over 40 — may have SLAP-type changes on MRI even without symptoms (Lansdown et al., 2018). That’s why accurate diagnosis is so important.
How Do SLAP Tears Happen?
There are two main types of SLAP tears:
- Traumatic: often from a fall, tackle, or sudden pull on the arm.
- Degenerative: from wear-and-tear or repetitive overhead activity, common in athletes and older adults.
A key contributing factor is posterior shoulder tightness, known as GIRD (glenohumeral internal rotation deficit). This restriction pushes the humeral head forward, increasing “peel-back” stress on the biceps anchor — one of the main mechanisms of SLAP injury in throwers.
Tests and diagnosis of SLAP Tears
Your physiotherapist may perform specific tests such as O’Brien’s, Biceps Load I and II, Speed’s test and the Compression Test. According to Hegedus et al. (2012), if at least 3 out of these 5 tests are positive, the diagnostic accuracy can be superior to an MRI.
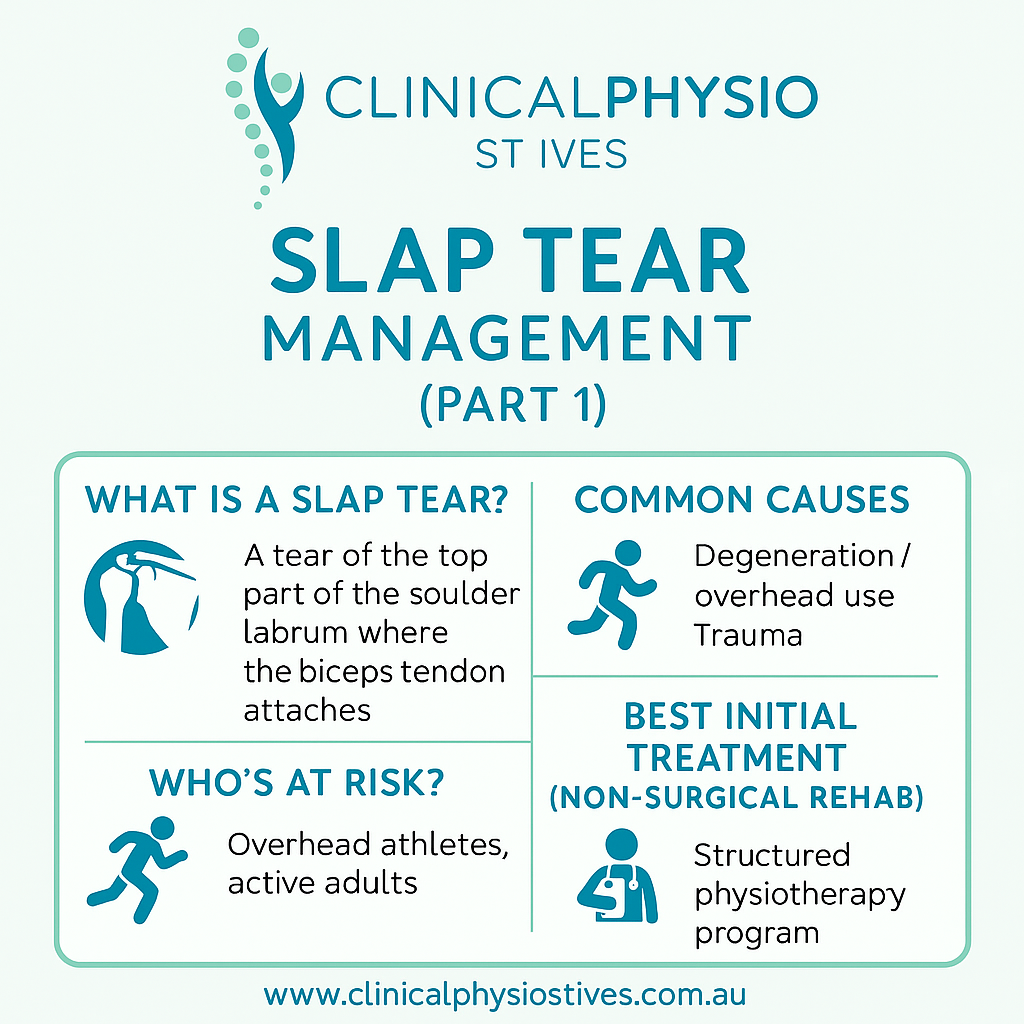
SLAP Tear Management and Rehab
The good news: most SLAP tears don’t need surgery. According to a 2025 consensus by Verma et al., first-line management should always be conservative physiotherapy — especially for non-traumatic or degenerative tears.
Rehabilitation focuses on:
- Restoring shoulder and spine mobility, especially internal rotation.
- Strengthening the rotator cuff and surrounding muscles.
- Stability exercises – these are especially important since the key role of the labrum is to deepen the otherwise shallow shoulder socket in order to increase stability.
- Improving neuromuscular control and scapular mechanics.
- Gradually reloading the biceps tendon with exercises shown to safely activate it (Cools et al., 2014; 2017).
A systematic review by Steinmetz et al. (2022) found that 78% of patients who completed a structured rehab program returned to sport or work — often within 5–6 months. Surgery is typically only considered if pain or instability persist after 3–6 months of dedicated rehab.
When is Surgery Needed?
For younger, high-demand athletes, or cases involving mechanical locking or instability, surgical repair may be appropriate. Research shows both SLAP repair and biceps tenodesis can be effective, though tenodesis tends to yield slightly fewer complications (Shin et al., 2021). Most athletes return to sport within 6–9 months post-surgery (Gregori et al., 2024).
Key Takeaway
SLAP tear management is rarely “one size fits all.” For most people — especially adults over 40 — a carefully guided rehab program with your physiotherapist provides excellent outcomes. Focus on restoring motion, building balanced shoulder strength, and progressing loading safely to return confidently to work or sport.