A Lower Back Stress Fracture, particularly in the lower lumbar spine, is a common overuse injury among athletes and active individuals. We explore lumbar bone stress injuries in depth, explaining their causes, how they’re diagnosed using advanced tools like stress fracture lower back MRI. We’re outlining effective pars defect treatment and lower back stress fracture rehabilitation strategies to support full recovery.
What is a Lumbar Bone Stress Injury (BSI)?
A lumbar bone stress injury (BSI) refers to bone microdamage caused by repetitive loading. It develops when the rate of microdamage exceeds the bone’s ability to remodel and heal.
Key Terms – They sound similar but are all very different!
- Spondylosis: osteoarthritis of the spine.
- Spondylolysis (pars defect): A non-displaced stress fracture of the pars; may be congenital/ hereditary, degenerative, isthmic, or pathological.
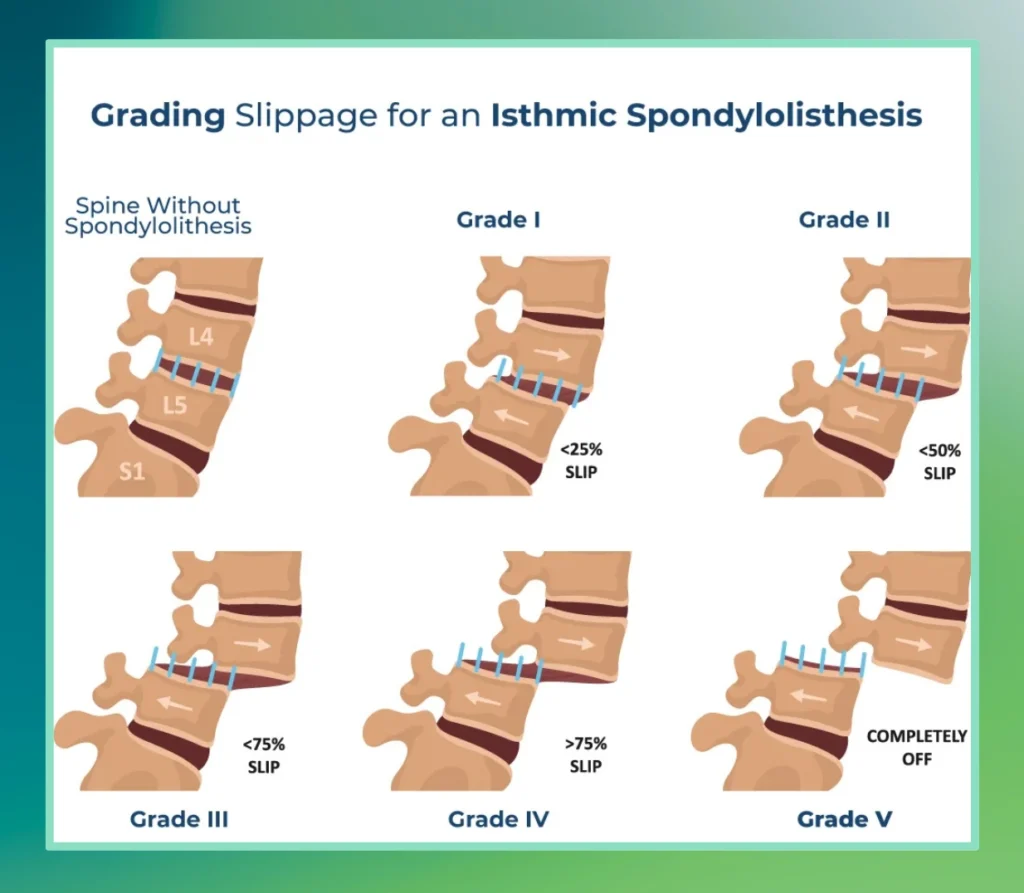
- Spondylolisthesis: Slippage of one vertebra over another, often caused by a pars defect. Isthmic spondylolisthesis is most common at L5/S1 and is graded by the Myerding classification.
Symptoms of a Stress Fracture in the Lower Back
In many cases, individuals with conditions such as spondylolysis or spondylolisthesis, which may involve or result from stress fractures, do not display any noticeable symptoms. When symptoms are present, lower back pain is the most common, and the condition is often only identified through imaging tests like X-rays or MRIs.
Stages of Lumbar Bone Stress Injuries:
- Bone Strain: Early-stage changes are visible on MRI or bone scans without symptoms.
- Stress Reaction: Visible bone stress on MRI with symptoms, but no fracture line yet.
- Stress Fracture: Clear fracture line on MRI, symptoms present, commonly referred to as a stress fracture in the lower back.
Anatomy of the Lumbar Spine: Where Stress Fractures Occur
Stress fractures in the lower back primarily occur in spongy (cancellous) bone.
The most common sites for lower back stress fractures are the Pars interarticularis and pedicle at L4 and L5 (80–95% of cases).
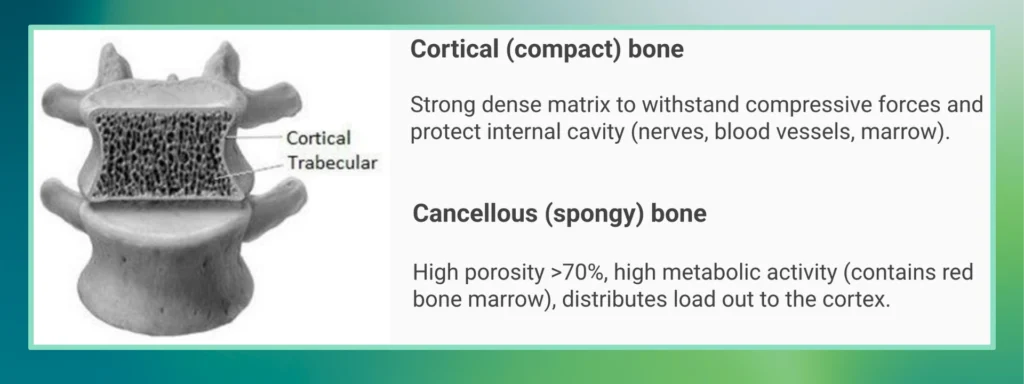
The lumbar vertebrae are composed of about 70% cancellous (spongy) bone, which heals more slowly than cortical bone. This makes the area more prone to injury and longer recovery. As shown in the image below.
How Bones Heal: The Bone Remodelling Cycle
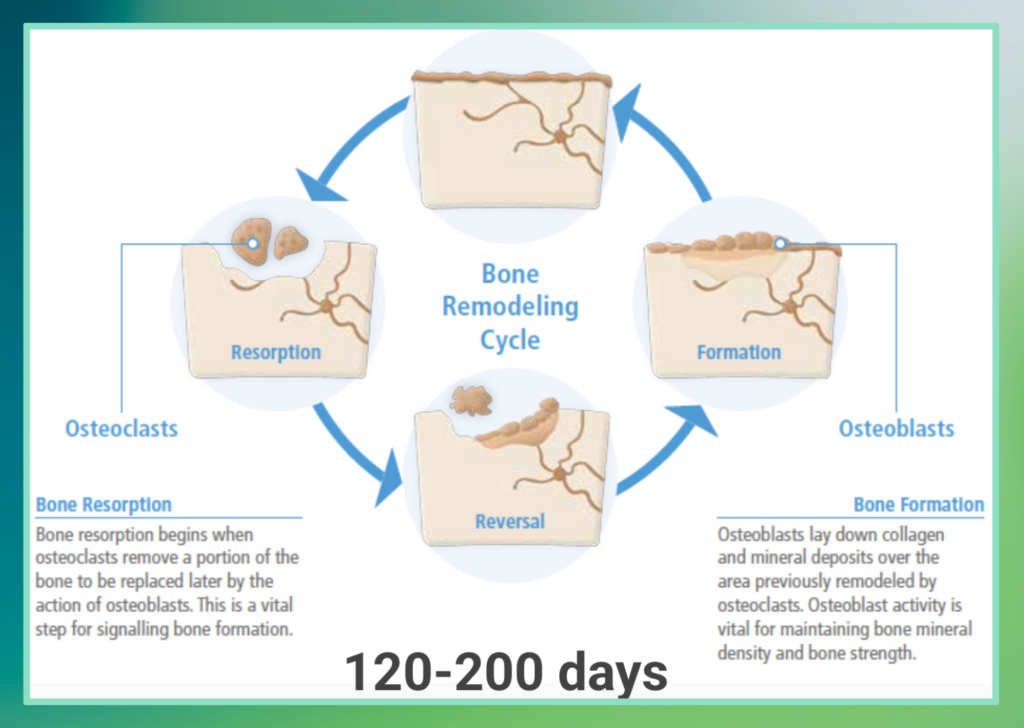
Bone remodelling is a dynamic process where old or damaged bone is continuously resorbed and new bone is formed to maintain both strength and mineral homeostasis within the body. This essential process is regulated by various factors, including genetics, hormones, nutrition, and physical activity.
Key aspects of bone remodelling include:
- Cells Involved: The process involves specific bone cells: osteoblasts (which form new bone), osteoclasts (which resorb bone), osteocytes, and bone lining cells.
- Bone Remodelling Cycle: This cycle consists of several stages:
◦ Resorption: Osteoclasts (Osteoblasts and osteoclasts are special cells that help your bones grow and develop) remove a portion of the bone. This step is vital for signalling bone formation.
◦ Reversal.
◦ Formation: Osteoblasts lay down collagen and mineral deposits over the area previously remodelled by osteoclasts. Osteoblast activity is crucial for maintaining bone mineral density and bone strength. - Duration: The full bone remodelling cycle typically takes between 120 to 200 days on average.
Bone stress injuries occur when the rate of microdamage formation exceeds the rate of this removal or replacement process (remodelling).
Why Do Stress Fractures Occur in the Lower Back?
Stress fractures occur in the lower back primarily due to a combination of repetitive mechanical stress, the specific anatomical composition of the lumbar spine, developmental factors in adolescents, and an imbalance in the bone remodelling process.
The Imbalance: A bone stress injury (BSI), which includes a stress fracture, occurs when the accumulation of bony microdamage outpaces this repair mechanism. In essence, new micro-cracks or damage are created faster than the bone remodelling process can repair or replace the affected bone tissue.
Lumbar stress fractures are especially common in sports with repetitive axial loading, extension, and rotation, such as cricket, basketball, and javelin.
- Cricket Fast Bowlers: Up to 67% lifetime prevalence
- Adolescent Risk: 23% incidence in youth bowlers due to incomplete spine mineralisation
The Adolescent Spine & Stress Fractures
The adolescent spine is particularly susceptible to bone stress injuries due to unique developmental characteristics. During puberty, bone accrual occurs at its fastest rate. However, increases in bone size typically precede increases in bone mineralisation.
This discrepancy between bone growth and mineralisation leads to a “fragility period“, where the spine may be more vulnerable to injury. Full bone maturity of the lumbar spine does not occur until 23-24 years old.
Despite this fragility, the adolescent spine also exhibits its greatest adaptability to mechanical load during these years, meaning axial and impact exercises can lead to greater increases in bone mineral density.
Risk Factors for Junior Athletes & Prevalence (in cricket)
Common in sports with repetitive axial loading, particularly into extension and rotation, e.g. cricket fast bowler, basketball, javelin. Typically, they have the following risk factors:
- Age 10-25 years old
- Sport Biomechanics
- Past history
- Low energy availability
- Training load/volume
Quick Stats:
- Cricket fast bowlers have a lifetime prevalence of lumbar stress fracture up to 67% (Johnson, Ferreira and Hush, 2012).
- Another prospective study showed 23% of adolescent fast bowlers develop an LSF (Kountouris et al, 2018).
- Most occur at the pedicle or pars interarticularis at L4 and L5 (80-95%)
Though Quadratus Lumborum (QL) asymmetry is sometimes mentioned, there are inconsistencies with some of the data. Current research shows that technique-related factors (e.g., shoulder–pelvis angles, side flexion) may be more important.
Diagnosing a Lower Back Stress Fracture
Diagnosis typically involves imaging, with MRI being the gold standard.
- Diagnosis includes:
- Subjective assessment (pain during sport, especially extension-based movements)
- Physical tests that involve extension and lateral flexion movement, like the single-leg hyperextension test and quadrant tests.
- Imaging, especially MRI, which is the gold standard for detecting stress injuries in the lumbar spine
Pars Defect Treatment & Lower Back Stress Fracture Rehabilitation
Most lumbar stress fractures respond well to conservative treatment. Surgery is rarely required.
The 3-Phase Conservative Approach:
- Protect Phase Weeks 1-6. Rest and symptom management. May include:
- Unloaded rehabilitation like pool running and cycling
- Low load lumbopelvic control and core exercises
- Avoid exercises that are provocative or may result in excessive or loaded lumbar extension/lateral flexion
- Protected Reloading Weeks 6-12. Gradual reintroduction of activity. May include:
- Strength training
- Gradual return to jogging/running
- Avoid high-intensity axial load
- Appropriate recovery with emphasis on sleep and nutrition
- Reassess
- Manage secondary risk factors
- Assess sport technique/biomechanics
- Transition to Sport Weeks 12-24. Structured sport-specific training and return. May include:
- Plyometrics
- Graded return to sport
- Appropriate recovery with emphasis on sleep and nutrition
- Reassess
Spinal Bracing – is it required?
- Not always necessary. Meta-analyses found that 83% of patients treated non operatively improved clinically regardless of any spinal bracing
- Used only if rest fails to alleviate symptoms.
- Can be removed once symptoms subside
Is surgery requried?
- Conservative, non-surgical outcomes: 92.2% return-to-play success
- Surgery rarely needed and depends on the grade of sponylolisthesis (slippage- see further info below)
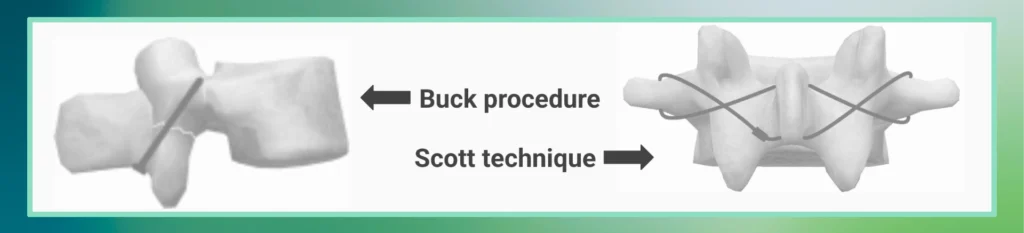
- Surgical options: Buck procedure, Scott technique (see image example below)
- Grades III & IV may require surgery if symptoms persist beyond 6 months
For adolescents, return to play (RTP) rates are high with both conservative (92.2%) and operative (90.3%) management (Overley et al., 2018).
What if there is a Slippage of One Vertebra Over Another?
The degree of vertebral slippage is classified using the Myerding classification, which has 5 grades based on the percentage of vertebral slippage visible on an X-ray relative to the vertebrae beneath:
- Grade 1: <25% slippage
- Grade 2: 25-50% slippage
- Grade 3: 50-75% slippage
- Grade 4: >75% slippage
Most patients respond well to conservative management, and surgical management is uncommon. Surgery is typically considered if conservative treatment has failed after more than 6 months.
Final Thoughts: Prioritise Early Diagnosis and Individualised Treatment
If you’re experiencing symptoms of a stress fracture back, it’s crucial to get an accurate diagnosis early. An evidence-based, structured rehab plan guided by a professional can significantly improve outcomes and help you return to sport or normal life with confidence.
Any information provided is informative in nature and not medical advice. You should book a consultation to discuss a 1:1 diagnosis and treatment with our team. Or contact your healthcare professional.
References:
- Hoenig T et al. Does Magnetic Resonance Imaging Grading Correlate With Return to Sports After Bone Stress Injuries? A Systematic Review and Meta-analysis. The American Journal of Sports Medicine. 2022;50(3):834-844. https://pubmed.ncbi.nlm.nih.gov/33720786/
- Johnson, G., Ferreira, P., & Hush, J. (2012). Lumbar stress fracture in cricket fast bowlers: A review. Journal of Sports Sciences, 30(10), 1033–1042. https://pubmed.ncbi.nlm.nih.gov/22261431/
- Kountouris, A., Sims, K., & Orchard, J. (2018). Risk factors for lumbar stress fracture in fast bowlers: A prospective cohort study. British Journal of Sports Medicine, 52(14), 884–890.
- Shah, S. A., Saller, J., & Scolnick, M. (2017). MRI classification of pars injuries. Current Sports Medicine Reports, 16(1), 10–15. https://www.ncbi.nlm.nih.gov/books/NBK545191/
- Fredricson, M., & Arendt, E. A. (2006). Classification and management of stress fractures. Clinical Sports Medicine, 25(1), 29–44. https://pmc.ncbi.nlm.nih.gov/articles/PMC4767832/
- Overley, S. C., et al. (2018). Return to sport after surgical and nonsurgical treatment for lumbar spondylolysis in adolescent athletes: A systematic review. Spine, 43(19), 1408–1416. https://pmc.ncbi.nlm.nih.gov/articles/PMC7809564/
- Institute for Spine & Scoliosis. (n.d.). Myerding Classification. Retrieved from https://www.spineandscoliosis.com.
- Xue, X., Wei, X., & Li, L. (2016). Surgical versus nonsurgical treatment for high-grade spondylolisthesis in children and adolescents: A systematic review and meta-analysis. Medicine (Baltimore), 95(11), e3070. https://doi.org/10.1097/MD.0000000000003070
- Scheepers, M. S., Gomersall, J. S., & Munn, Z. (2015). The effectiveness of surgical versus conservative treatment for symptomatic unilateral spondylolysis of the lumbar spine in athletes: A systematic review. JBI Database of Systematic Reviews and Implementation Reports, 13(3), 137–173. https://doi.org/10.11124/jbisrir-2015-1926
Lower Back Stress Fracture FAQs
Lumbar vertebrae are composed of approximately 70% spongy (cancellous) bone. This is significant because spongy bone has high porosity (>70%) and high metabolic activity, containing red bone marrow and distributing load to the cortex. Crucially, spongy bone takes longer to heal than cortical bone, impacting recovery times for injuries in this area.
The full bone remodelling cycle, a dynamic process where old or damaged bone is continuously resorbed and new bone is formed to maintain strength and mineral homeostasis, takes approximately 120-200 days on average. This cycle is regulated by genetics, hormones, nutrition, and physical activity, involving cells such as osteoblasts, osteoclasts, osteocytes, and bone lining cells.
Full bone maturity of the lumbar spine typically occurs at 23-24 years old. This period is critical for bone development, as bone is accrued at its fastest rate during puberty.
The “fragility period” refers to a discrepancy in bone growth and mineralisation that occurs during adolescence. While bone size increases, bone mineralisation lags, making the spine more susceptible to stress injuries. Despite this, bone also shows its greatest adaptability to mechanical load during these years, meaning axial and impact exercise can lead to greater increases in bone mineral density.
True. According to the sources, 80% of spondylolysis (specifically isthmic spondylolysis, which results from a pars defect) is asymptomatic. Spondylolysis is defined as a non-displaced stress fracture of the pars interarticularis.
For both lumbar bone stress injuries (BSIs), including spondylolysis, and lower-grade spondylolisthesis (Grade I & II), management is primarily conservative. Most patients, particularly adolescents, respond well to conservative management.
Conservative Management for BSIs/Spondylolysis: This typically follows a progression of “Protect” (rest/reduced activity), “Protected reloading” (gradual increase in activity and load), and “Transition to sport.”
Conservative Management for Spondylolisthesis: Grade I & II spondylolisthesis are treated similarly to spondylolysis. Treatment for Grade III & IV remains controversial. Surgery is generally considered only if conservative treatment has failed for more than 6 months.


